Everyone loves technology, but it can drive us crazy when technology-led transformation implementation doesn’t support better patient care outcomes.
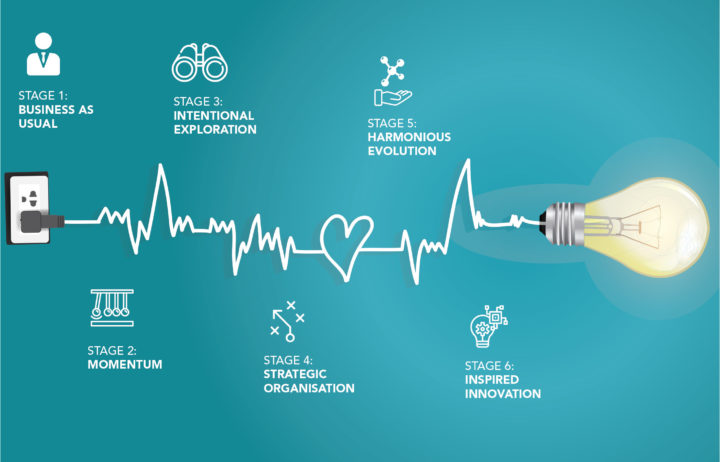
We partner with healthcare organisations in their transformation and to implement their strategies and goals and inevitably these initiatives include buzz phrases like “becoming tech-enabled” or “actively investing in tech.” Translated, this means investment into new tools, platforms, software, and services, primarily to drive efficiency and practice change.
Communication Void
For patients, the time between making the booking and the visit is often a communication void where patients feel uncertain or do not feel informed because they haven’t retained the information relayed to them about their appointment.
These feelings contrast with patient expectations.
Emboldened by experiences in other industries, patients are demanding a more interactive and engaging experience during their healthcare. Further, these increasingly digital-savvy patients, or even digital native patients, have an expectation that technology will not only provide access to online healthcare bookings, but that it will also support:
- delivery of personal appointment reminders and instructions;
- management of appointments online;
- notifications of appointment delays; and
- instant access to health records and test results.
By understanding patients’ experience expectations, we can now integrate technology into the transformation to reshape the experience and deliver better patient outcomes.
Opportunities to Engage
Each of these new digital interactions is an opportunity to engage with patients ahead of their visit and provide enhanced communication which will have a positive impact on their compliance with their appointment instructions.
Additionally, engaging patients ahead of their visits provides new benefits including:
- Reducing feelings of anxiety and stress related to the appointment through introducing the friendly practice team.
- Minimising anxiety about finding the location of the practice and arriving on time by providing a map with information about parking, disabled access, and public transport.
- Increasing familiarity prior to arrival at the practice by providing a link to a digital ‘walk through’ related to your appointment.
- Providing a checklist of information to bring to the appointment.
- Priming patients to make a list of topics they hope to discuss during their next phone conversation or practice visit.
- Providing the name and phone number of a practice representative in case they have questions.
- Managing upcoming appointments by providing after-hours access or a contact if patients need to change appointment times outside of practice hours.
- Setting the expectation that the next communication or appointment is an opportunity to discuss and interpret information together.
- Notifying patients of appointment delays prior to their arrival.
- Explaining what happens next.
At Experience 360, we have seen the positive outcomes of this engagement first-hand.
For many of our clients, adopting these more dynamic communication approaches to pre-appointment engagement is paying off. For example, practices that have deployed automated SMS or email appointment reminders, are seeing patient no-show rates go down by nearly 20 percent and, as such, they are recuperating costs in the tens of thousands.
The Biggest Gains Through Transformation
For our clients, the biggest gains in technology-led transformation may come from helping healthcare professionals and patients to share information and communicate more effectively. By applying a patient-centred approach, they have solved many other practice communication challenges such as:
- Improving patient-practice communication, between booking and appointment, to reduce no-show rates.
- Increasing adherence to post-procedure and/or wound care instructions to cater for recovery and care management instructions to real-time patient needs.
- Creating two-way communication for on-going care and pain management plans to reduce patient concern.
- Providing an integrated care environment to encourage collaboration (between patient and health professionals) to support continuity of care for patients with chronic conditions.
- Developing two-way alerts to support adherence to care management programs.
- Incorporating dynamic approaches into care programs to improve medication, health, and care adherence.
- Personalising instructions and medical records to encourage patients to participate and better manage their own care.
- Increasing adherence to pre- and/or post-hospitalisation instructions to improve recovery times, increase patient satisfaction, and reduce post-hospitalisation and post-surgical complications.
- Sharing pre-surgical instructions specific to each patient’s procedure and comorbidities rather than generic instructions for all operations.
- Incorporating telehealth consultations into the care journey to increase convenience and decrease dependence on practice visits.
How do we Implement the Right Technology in Transformation?
But how do we know we are implementing technology in transformation in a way that is engaging for patients and improves their experience?
By putting patients in the driver’s seat.
Up until now, patient engagement technologies have included patient portals or secure messaging tools. These technologies, however, have left the patient beholden to the provider. Although certainly intended to make healthcare more convenient and patient-centred, they actually create more work for patients.
Take, for example, the patient portal. Most practices adopted the patient portal just for the sake of offering a new technology tool as opposed to designing a tool with features that would truly benefit their patients. For patients, however, a portal is not necessarily a great experience; it can be difficult to navigate and they have to remember the password!
Patient portals often lack functionality and personalised information and the data does not always have the context necessary to spur patients to action. Nor do they provide real-time updates. Imagine you are a patient trying to manage your chronic disease and you need to continuously log in to access your information. It is a massively manual process because the portal requires the patient to action something. It is one more burden to the patient in their healthcare.
Contrast that experience with new patient engagement technology which is centred on activating patients to take charge of their own care management (putting patients in the driver’s seat) and driving home the notion of patient-centred healthcare. This directly aligns with patients who are demanding a more interactive and engaging experience in healthcare as they become emboldened by their experiences with other business sectors.
However, we are not there yet. We need to push further beyond generic information and into personalising the experience and responding to individual patient’s needs. Additionally, these improved concepts are not likely to be inside a portal and instead would be customised to how patients want to receive their information.
Think about how we receive information today. Regardless of age, we all have a mobile phone in our hand. Translate that to communication between patient and a healthcare practice by considering that patients are more likely to access tools conveniently located on their smartphone instead of a less operable portal.
This consideration and view provide a great opportunity for technology to assist in delivering a personal, convenient, and interactive patient-centred solution.
Conclusion
Looking at transformation experiences in other industries, combined with emerging technologies and changing patient behaviours, are driving a shift in what patients expect from their healthcare practices.
To keep pace with changing patient demands, practices must adopt a more dynamic patient-centred communication approach, designed to promote information sharing, reduce patient burden, and truly deliver on the notion of patient-centred care.
The biggest gains for patients, and the quickest wins for practices, do not come from making massive digital changes. They come from finding opportunities to improve communication between patients and practices. Despite business pressures, efficiency imperatives, and time constraints, big wins can be achieved when healthcare professionals and patients communicate more effectively with each other.
Technology-led transformation and communication will play a crucial role in supporting the transformation of patient experiences. Together, they will change the way practices work, increase the value of care, and essentially focus the business on the people who determine practice success – our patients.
Not such a bad idea, is it?
To find out how Experience 360 can help you on your transformation journey to a patient-centred care model, contact us today.