Technology is an ever-increasing component in improving the patient experience. But exactly what role does technology play when an organisation is transforming to a patient-centred care model?
Everyone loves technology, but it can drive us crazy when technology-led transformation implementation doesn’t support better patient care outcomes.
We partner with healthcare organisations in their transformation and to implement their strategies and goals and inevitably these initiatives include buzz phrases like “becoming tech-enabled” or “actively investing in tech.” Translated, this means investment into new tools, platforms, software, and services, primarily to drive efficiency and practice change.
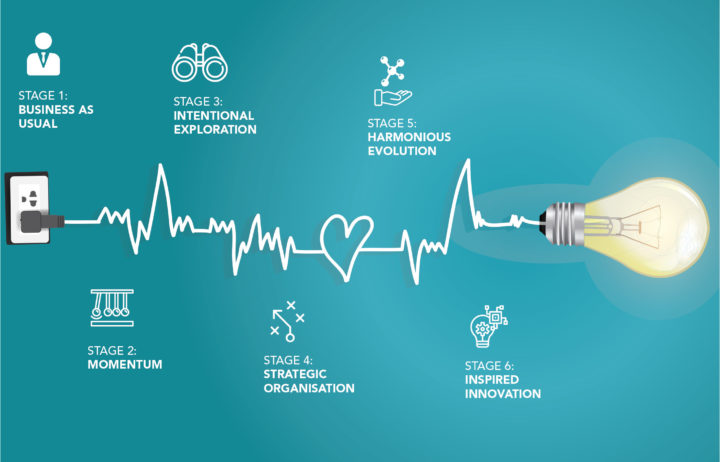
Transformation – The Order Is Wrong.
In our opinion, compared with true transformation models, these technology-led improvements are ordered backward.
For practices, the concept to date has been ‘if we build it, they will come’. The expectation of implementing technology in transformation has been to drive efficiency, reduce overheads, and get access to data. Unfortunately, many of these expectations remain unrealised and the patients largely have not arrived.
Practices also had an expectation that technology would improve the patient experience through seamless data access, care management, and patient activation in care. Instead, so far, it has largely left them dissatisfied with technology that is inconvenient, inconsistent, and not personalised.
Further, while technology should play a pivotal role in transformation and the modernisation of healthcare practices, it often complicates rather than supports integrated patient-centred care. Technology is just a tool and the automation of broken service-delivery processes only gets you more efficient broken processes.
The Right Order in Transformation.
So, how do we incorporate technology, increase the value of care, improve outcomes, and efficiency while at the same time producing practice growth?
By flipping our mindset and putting the patient at the centre of the transformation process!
Patient-centred transformation orders change in a practice differently. You first determine the patient outcomes you want to achieve (purpose), then rework the business functions, processes, and technology to achieve your goals.
This is a process in which consideration and integration of technology is driven by purpose and that purpose reshapes the business to produce better patient outcomes.
In this two-part blog, we discuss how the everyday scenario of scheduling appointments is impacted by technology and communication, both for patients and the practice, and how better patient care can be achieved.
Non-Compliance with Appointment Instructions.
It is not uncommon for patients to turn up to a practice without having followed instructions. The consequence is that they need to be rebooked, which causes disruption to schedules, delays appointment availability for other patients, and impacts practice productivity and revenues.
Further, while the impact of these non-compliant patients varies depending on the type of practice (GP, pathology, imaging, specialist, allied health), the quantum of patients requiring pre-appointment preparation and the relationship between preparation and its effect on patient outcomes (fasting, bowel preparation, biopsy, medication, attire) can be significant. The impact to the practice is further compounded by no-shows and last-minute appointment rescheduling.
The revenue impact to the practice can be a loss in the order of one-tenth to one-third.
Therefore, our desired outcome (purpose) is to maximise patient compliance with appointment instructions and to minimise frustration, inconvenience, and loss of time for everyone.
In our experience, when patients do not comply with appointment instructions, it is usually a symptom of a more widespread problem within your practice.
Research indicates most barriers to patient compliance are created by healthcare professionals themselves. You may be completely unaware that you, and your practice team, create these patient failure points in your practice every day. They are largely created by ineffective communication.
Three hot spots that cause patient compliance failure.
Let us consider how and why patients fail to comply with appointment instructions.
Patient instructions usually originate from the doctor but are often relayed to patients by another member of the healthcare team. The process of delivering this message — from the doctor, via one or more members of the team, to the patient — is a bit like the game of Chinese Whispers.
The more people the message is relayed to, the more likely it is to contain errors by the time it reaches the patient. The resulting patient instructions do not reflect or deliver the doctor’s intent.
Within this flow of communication, there are three hot spots of communication failure which all lead to non-compliance. Each of these failure points occurs during communication between the patient and the healthcare team delivering the appointment instructions.
The root cause of patient non-compliance is nearly always communication failure on the part of the practice team in one or more of the three hot spots. These hot spots are:
- No Instructions – The patient was not given any instructions at all. This is the most obvious failure.
- Misinterpreted Instructions –The instructions were not clear to the patient and, as a result, were misunderstood or misinterpreted. This is the most common failure.
- Method of Communication is Not Working – The method of communication did not support the patient and enable them to easily follow instructions e.g. digitally illiterate patients receive appointment information via email or SMS. This is the most misunderstood failure.
Based on our work with many different healthcare practices, the root cause of patient non-compliance is nearly always communication failure on the part of the practice team. You can easily confirm this for your practice through a detailed discovery process.
Solving this problem.
Solving this problem is centred around improving patient-practice communication.
Today, medical appointments can be made via online booking, the phone, or face-to-face. The patient experience related to each method should be documented and scrutinised to identify communication hot spots and obstacles impeding patients to comply with appointment instructions.
Phone and face-to-face bookings are the most manual processes and have the highest likelihood of failure as they rely on the communication skills of both the patient and the practice representative. This is, therefore, a higher potential source of patient non-compliance with appointment instructions.
In contrast, online booking methods experience much higher patient compliance outcomes because the booking process can be automated. Simple and easy; provided the correct communication is sent!
Let’s dig into this a little deeper.
During phone and face-to-face booking methods, the appointment instructions are relayed to the patient verbally. This creates a bigger challenge because the patient is listening to the instructions, but most patients are unable to interpret (think) or write as fast as the practice team member is speaking.
This can be explained by understanding human interaction speeds.
In his book Human Performance Engineering, Robert W. Bailey indicates that most of us speak at the rate of about 125 words per minute. We have the mental capacity, however, to understand someone speaking at 400 words per minute (if that were possible).
This difference between speaking speed and thought speed means that, when we listen to an average speaker, we are using only 25% of our mental capacity. As a result, patients need to make a real effort to listen carefully because, if they do not, their minds turn to other thoughts.
During a stressful healthcare conversation, it is highly likely the patient’s thoughts could be jumping to the worst possible outcome (it’s human nature to think the worst) and their ability to listen carefully to instructions will almost certainly be impaired.
In circumstances where people’s listening is inefficient or impaired, the average listener hears, understands, and retains only 50 percent of what was said. Within 48 hours, that retention drops off another 50 percent to a final level of 25 percent efficiency. This is not an optimal outcome when a patient is listening to pre-appointment medical instructions.
To improve information retention when instructions are being relayed over the telephone, patients may choose to write the instructions down. Unfortunately, research does not support writing instructions. An article published in the Journal of Experimental Psychology titled Adapting To Processing Demands In Discourse Production: The Case Of Handwriting indicates writing slows our human interaction speed. On average, we write at only about 31 words per minute (when memorising) which even further reduces a patient’s ability to accurately capture the instructions.
Regardless of the booking method, the highest likelihood of patient compliance success is to provide patients with written confirmation of their appointment instructions so they may read and refer to them prior to the visit.
In Part Two of this blog, we look at the gap between booking appointments and office visits and how technology can support patient-centred outcomes.